Mr. Smith is an elderly resident of a long term care facility with atrial fibrillation. He’s been taking Coumadin for years for stroke prevention and was just recently hospitalized for pneumonia. His Coumadin dose was decreased in the hospital due to a drug interaction with an antibiotic, and he was discharged back to the nursing facility on this new lower dose. While he was out of the facility, he missed his routine lab draw for his Coumadin. Within the week, Mr. Smith has returned to the hospital after suffering a stroke since his Coumadin dose was sub-therapeutic.
This is a nightmare scenario for the resident, their family, the hospital, and the nursing staff. Unfortunately, transitions of care in our healthcare system leave much to be desired. Our residents are on complicated medication regimens often treating numerous disease states. Even with the rise of electronic health records and multiple electronic messaging platforms, it is still difficult for different healthcare providers to piece together the whole story.
Long Term Care Rx’s goal is to help prevent situations like Mr. Smith. Studies have found that adverse drug events attributable to medication changes occurred in 20% of transfers between nursing homes and acute-care hospitals. One-third of these events were considered preventable (AMDA Transitions of Care CPG, 2010). If your facility accepts five admissions or readmissions a week, the statistics point to at least one of those admissions will lead to an adverse drug event due to a medication change. That’s fifty-two medication errors a year in population that is high risk due to age and multiple medications used concurrently. Over seventeen of those errors are considered preventable. That’s seventeen fewer adverse effects, hospitalizations, or even deaths. It’s statistics like this that reinforce how important this transitions of care program can be and what type of impact it can have clinically.
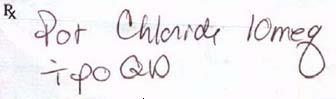
Assisting in these transitions of care has been a major point of emphasis for the Long Term Care Rx pharmacy team over the last 12 months. Within 3 business days of every admission or readmission to a skilled nursing facility, a member of our team tries to put together all of the puzzle pieces to make a complete picture of that resident’s healthcare. We take a look at previous medications prior to the level of care change, assess why the level of care changed, and ensure that the ideal medication regimen is being provided to each resident based on his or her needs. We look for new drugs, especially new drugs that commonly result in adverse effects, and make sure the nursing facility is aware of what needs to be monitored. Our goal is to make sure that residents stay at your facility and reduce hospital readmissions.
We encourage all of our facilities to take advantage of our transition of care program. With your help, we can be proactive and catch any issues before they progress into problems. If you have any questions regarding our transitions of care program, please don’t hesitate to contact the pharmacy directly for more information. With your help, we can be proactive and catch issues before they progress into problems. Together, we can ensure the best possible care for each and every resident.
Drew Curtis, PharmD
Pharmacist Manager
Consultant Pharmacist